[
] 219
R
isk
G
oveRnance
and
M
anaGeMent
ronment of the last few weeks. This means that human adaptability to
continuously changing weather conditions, and thus the variability of the
regional climate, is taken into account. It is important to consider short-
term adaptation because the human body reacts differently to its thermal
environment due to physiological adaptation (short-termacclimatization),
which augments the efficiency of the thermal regulatory system and thus
reduces the thermal load effectively acting on an individual. In addition to
this, short-term behaviour-based adaptation – such as changing clothes
–can reduce the thermal stress acting on the individual. Therefore, epide-
miological studies find lower thresholds for which heat affects human
health in colder climates than in warmer climates, as well as for the begin-
ning of the summer season compared with the end.
DWD calculates the ‘perceived temperature’ in order to assess the
thermal environment of the human being. The perceived temperature is
determined through a simple heat budget model of the human organism,
which includes the main thermophysiologically relevant mechanisms of
heat exchange with the atmosphere. The most important meteorological
parameters included in the model are: air temperature, humidity, wind
speed and radiation fluxes in the short-wave and long-wave ranges. The
short-term adaptation approach is then used to adjust the threshold upon
which a warning is issued. This depends on the meteorological situation
of the past few weeks within a certain range. The thermal load category is
then determinedwith the perceived temperature forecast for 12 UTCused
for the evaluation of heat and the perceived temperature forecast for 06
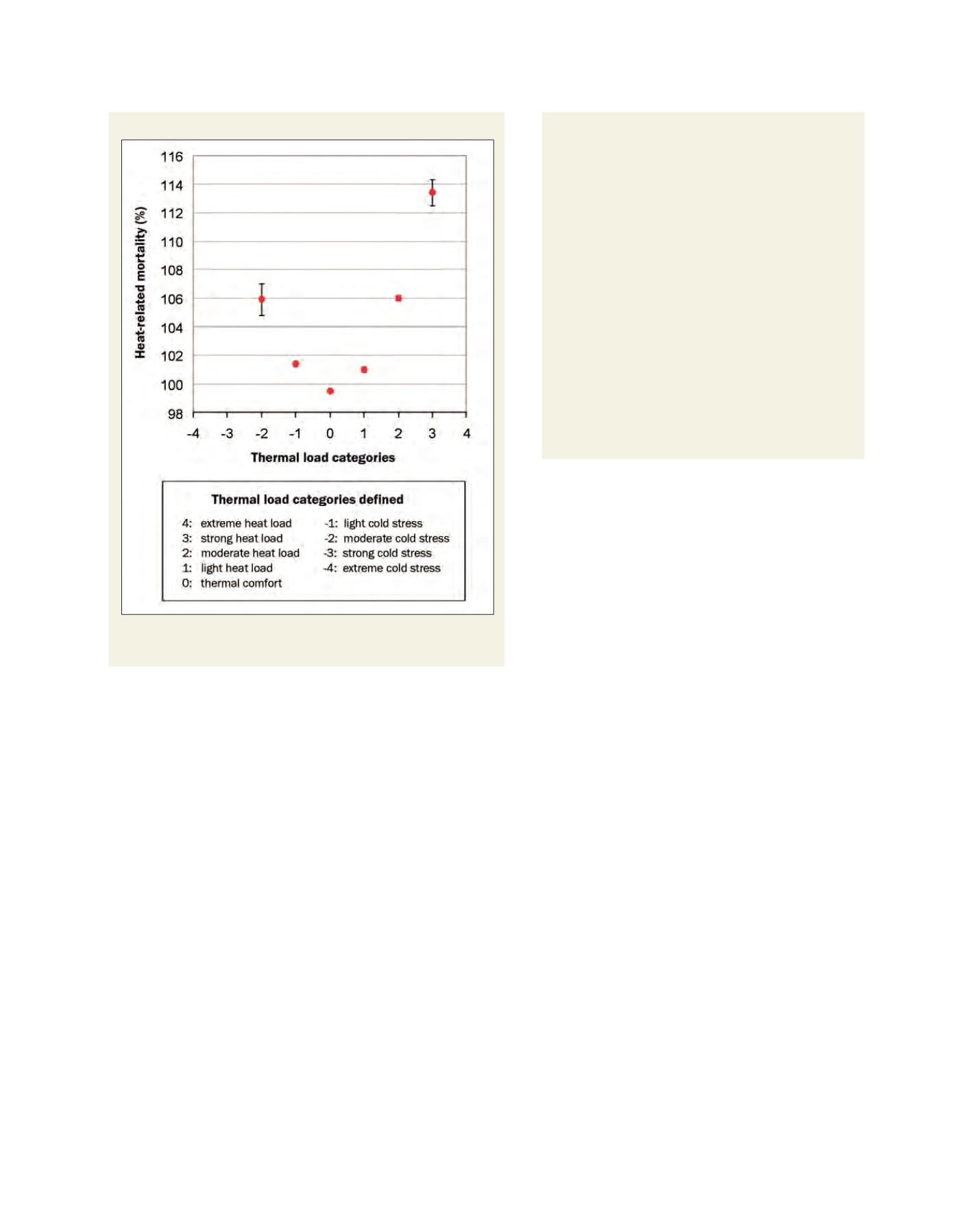
Heat-related mortality comparisons
Heat-related mortality in comparison to the expected total mortality rate (all age
groups) for different thermal load categories in Baden-Württemberg (1968 – 2003)
Source: C. Koppe, 2005
UTCused to determine cold. During situationswith at least a
moderate heat load (cold stress) totalmortality is significantly
increased.
4
In order to avoid too many warning situations
per year in Germany, a heat warning is issued if a strong or
extreme heat load is forecasted –where a mortality increase
of more than 10 per cent is expected.
As well as the daytime heat, the HHWS in Germany also
takes night-time air temperature into account. A warning
will only be issued if the night-time temperature does not
fall below the 95th percentile. This additional criterion was
included because the main target of the German HHWS
is the elderly living in nursing homes. Therefore, it is
important to include an indicator for the nocturnal cooling
potential of indoor conditions. To get a better indication
of the indoor environment a thermal simulation model for
buildings was also added. This information is considered
before the biometeorologist decides whether or not to issue
the heat warning suggested by the model. The warning is
then disseminated via the internet to the general public and
by email and fax directly to care homes – as well as to the
health authorities of the Bundesländer, who may decide to
place it on the radio and TVprogrammes of the public chan-
nels. The advice given during a warning depends on the
local health authorities, but targeted advice is usually given
to the general public and to institutions that take care of the
elderly or disabled, such as nursing homes. An evaluation
of the HHWS in the State of Hessen has shown that hospital
admissions due to heat related disorders fromnursing home
inhabitants have decreased significantly since the introduc-
tion of the HHWS.
5
A precondition for the optimization of a HHWS is that
the system is adapted to national, regional and local require-
ments. These can differ in space and time, even when only
considering the meteorological component. Therefore, it
would be wrong to conclude that one system is superior
to another. Countries that plan to implement or revise a
HHWS have to follow local needs.
Heat advice for the general public
and for nursing home staff
Advice to general public:
• Wear light, loose-fitting clothes
• Drink at least 2-3 litres of water a day
• Avoid alcohol and drinks with caffeine
• Eat only light meals
• Avoid strenuous physical activity
• Stay in the shade
• Wear a hat
• Restrict physical outdoor activities to early morning or evening
• Do not waste water.
Advice for nursing home staff:
• Check room temperatures and if necessary try to cool the room
• Take care that patients drink sufficient water or other liquids
that contain sufficient minerals in order to avoid dehydration.
Be aware that some patients need to be helped to drink
• Check clothes and blankets
• Look for signs of dehydration or other illnesses
• Reguarly check those who can’t care for themselves. Make a
drinking plan and measure body temperature if necessary
• Call the GP immediately if health status deteriorates.
















